Overview
Hospital mergers and acquisitions are happening at a dizzying rate, and that means intense change for employees of those systems, from expanded patient services to leadership upheaval.
But for those working in HIM and HIT, the biggest impact of M&A activity comes from merging EHR systems. In doing this critical work, health information professionals must ensure that patient data is preserved, deduplicated, and made available in all corners of the enlarged organization.
That’s why it’s important for health IT and revenue cycle leaders to understand the EHR migration challenges that come with mergers and acquisitions, and how they can preserve data integrity in two essential ways: through master patient index (MPI) cleanup and clinical data abstraction.
Download Preserving Data Integrity During Epic Migration: A Tale of Two Systems, and learn how you can preserve data integrity and overcome data migration challenges.
About e4health
e4health is a trusted provider of health information management and healthcare information technology solutions that deliver value-based outcomes across today’s complex landscape.
Our solutions offers flexible end-to-end solutions that address revenue cycle management and data quality issues that health networks, hospitals, outpatient providers, and physician practices rely on to improve quality, overcome challenges, and drive better outcomes.
Utilizing strategic partnerships and proven methodologies, we combine leading-edge technology and best practices to elevate the business of healthcare and impel value and quality throughout healthcare organizations across the nation.
e4health Trusted Solutions

M&A Overview
Migration Challenges with Mergers and Acquisitions
Although Kaufman Hall reported slightly fewer M&A transactions during the height of the COVID-19 pandemic, it’s once again on an upswing. In fact, total revenue from hospital and health system mergers and acquisitions during the second quarter of 2022 far exceeded that of any prior year’s second quarter, according to Kaufman Hall’s latest industry report.
Kaufman Hall suggests two reasons for the uptick in M&A activity. First, hospitals need to find partners that can help them in the continued evolution of healthcare, including growth in outpatient services, telehealth programs, and home healthcare. Second, smaller hospitals that face financial challenges may see it’s no longer viable to stay independent and may need partners.
The American Hospital Association lists three technology benefits of mergers:
- Expanded repositories of clinical and cost data
- Real-time support of diagnoses and treatments
- Advanced analytics
EHR Migration Challenges: Preserving Data Integrity
Scenario 1: MPI
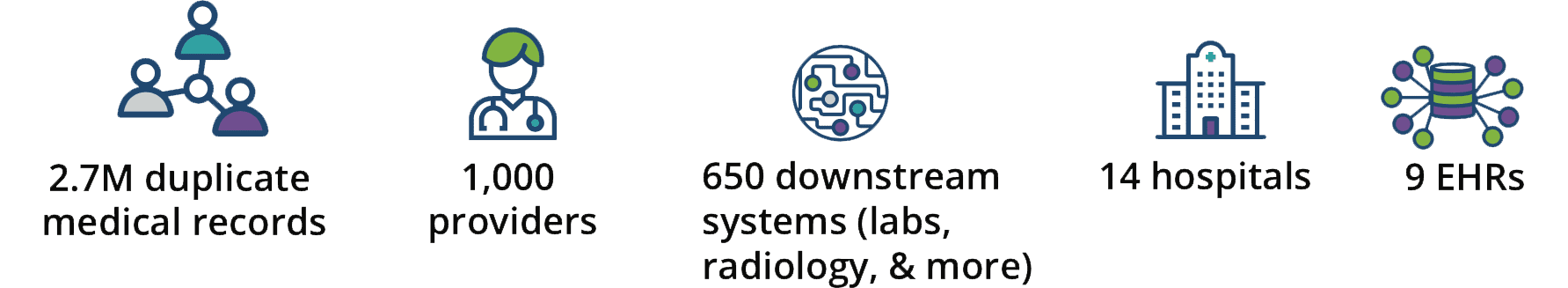
A NJ-based health system was tasked with migrating Epic into 14 hospitals and 1,000 providers. There were nine different EHR systems and approximately 650 downstream systems including labs, radiology, respiratory, and more. The leadership team had to create a strategy to tackle all their disparate systems and duplicate patient information across facilities.
Scenario 2: Abstraction and Validation
A Midwest health system used a local staffing agency for the first 2.5 years of Epic go-live but couldn’t afford to keep temp employees in-house. With more acquisitions, they experienced larger time gaps moving from one project to the next. They needed a different data abstraction strategy, and fast.
Health IT leaders must carefully consider the financial, organizational, and clinical costs with Epic migration. Here’s how two organizations made the most of master patient index cleanup, data abstraction, and validation.
Tale One: Preserving data integrity with MPI cleanup
Background
Epic EHR is the engine that drives patient care, operational decisions, and contextual insights with reliable, holistic, and integrated data for a health system and its affiliates. But importing millions of patient records from multiple data sources into a single EHR creates enterprise- level overlaps. Overlaps must be merged into the enterprise master patient index (EMPI) to ensure system integrity and manage critical patient care implications.
In this case more than 2.7 million overlaps had to be addressed.
Each facility also had same-source, facility-level duplicates that demanded resolution before addressing the enterprise-level overlaps.
Goals
< 3% – Patient identity integrity is so crucial that Epic requires a duplicate rate of 3% or less before an enterprise can “go live” with Epic. Given the considerable investment in Epic and the fact that high-quality data is among the most valuable assets to the organization, an MPI cleanup was central to the system-wide comprehensive data migration project.
9 months – The health network aimed to reduce the time frame and manual effort needed to address millions of potential overlaps and facility- level duplicate records.
Quick Facts + Impacts
Preserve data integrity with MPI execution in three areas:
1. Resolve enterprise overlaps and same- source duplicates: This was done in patient populations of each legacy system. Next, the team deployed referential matching technology, identifying 70% of enterprise overlaps, and matching same-source facility duplicates. Finally, the resulting data was used to verify each matched case, merge the records, and address the impacts on downstream systems.
2. Determine surviving records/targets: A surviving record/target is the designated “source of truth” into which all data for a patient is merged. First, the team built a customized merging algorithm using health system-defined parameters. The algorithm was based on a weighted record hierarchy. Factors used to determine the algorithm were number of visits, most recent visit dates, oldest registration dates, and records that exist in specific downstream systems. Then, a highly trained team used the algorithm’s specific enterprise and facility rules to determine target records.
3. Merge downstream systems: This effort involved a detailed decision flow process to ensure that all downstream systems were accounted for and appropriately matched with the EHR and EMPI. Project leaders considered each facility, each ancillary system within that facility, and whether the downstream system overlapped across multiple facilities within the enterprise.
Project Results
- Reconciled enterprise-level overlaps
- Resolved same-source, facility-level duplicates
- Merged and/or validated 650 downstream systems
- Created a structured and sequential rules-based process
- Delivered within the tight 9-month time frame
- Reduced duplicate rate to 2.5%, below Epic go-live goal
Considerations for legacy EHR integration
Interfacing legacy systems into a new Epic EHR platform is not an exact science. Legacy systems often have significant limitations, making all- inclusive interface matches a challenge. This can result in data loss, duplicate records, and the inclusion of non-pertinent data. Failure to consider these challenges can result in data that is inaccessible, inaccurate, and inappropriate in the new EHR system.
That’s what happened when the Department of Veterans Affairs migrated its system to a new Cerner EHR, according to a Government Accountability Office report. The government watchdog concluded that the VA didn’t ensure the quality of all the data it was migrating because it did “not establish and use performance measures and goals.” Because of this oversight, the migration was plagued by problems such as clinician confusion about what data was available, data inaccuracy, and cluttered and irrelevant data.
Key role of physicians and how to bridge satisfaction and reduce burnout
Though the job of migrating an EHR system falls to the HIM and HIT teams, the end users will be physicians. That means physicians will play a key role in how the migration unfolds as well as the aftermath to ensure their satisfaction with the end result. If the data migration causes additional physician fatigue, as it did for the VA, there’s a problem. Instead, migrations should proceed with uninterrupted access to quality and complete patient data to ensure minimal disruption to patient care flow and physician process and productivity.
Tale Two: Preserving data integrity with MPI cleanup
Background
WellSpan, a large health system in Pennsylvania, needed to consolidate its five legacy EHRs and convert the entire system to the Epic EHR platform within three years at a cost of $188.7 million. Physician satisfaction was essential.
Goals
- Capture all critical clinical data
- Eliminate duplicate or unnecessary data
- Ensure seamless access without interruption for clinicians on day one of patient visits
Preserve data integrity with clinical abstraction in three areas:
1. Create a preload strategy:
The team decided to preload 250,000 records of patients who were anticipated to have appointments in the next six months and patients who had multiple appointments within the past 18 months. Using this strategy, key patient information was preloaded into Epic prior to the patient visit, allowing for continuity of patient care.
2. Employ clinical abstractors:
A team of experienced clinical data abstractors reviewed all interfaced data, eliminated duplications, added uninterfaced key clinical data elements, and performed a comprehensive validation to ensure that each patient record was accurate and ready for use on day one.
3. Use a joint staffing approach:
In addition to engaging health system employees who worked hours outside of their typical schedules, the vendor partner supplied clinical data abstractors who ramped up and down as the workflow dictated. When a newly acquired cardiology practice was part of the integration, a clinical data manager worked with the practice to identify their distinct key clinical data elements and meet their specialized needs.
Abstraction and validation working in concert:
The clinical data manager, the cardiology practice manager, and the group physicians identified and tailored key findings that the physicians deemed essential for inclusion in the EHR.
Project Results
- 250,000+ patient records converted to Epic EHR
- 99% accuracy throughout the clinical data migration to Epic
- 53% increase in efficiency as the project progressed
- 233% increase in abstractor staffing with experienced, precise personnel
- 10,000 records scanned and abstracted for cardiology practice in four weeks
Not All Epic Migrations Are Created Equal
There’s a lot on the line during an Epic migration: It can take years, cost millions of dollars, and put patient safety and physician satisfaction at stake. That’s why it’s crucial for health systems to work with trusted partners to ensure their efforts are successful.
With e4health, health systems can trust that expert people, processes, and technology are at the helm of this crucial work. MPI cleanup includes a team of full-time MPI specialists with investigative and decision-making skills to deliver timely remediation and cost-effective, large-scale duplicate record identification and resolution.
In addition, experienced data abstractors ensure smooth transitions from paper charts and legacy systems to new EHRs. Physician practice and clinic records are abstracted from multiple sources. Data is input according to practice-specified clinical data elements including medication lists, problem lists, progress notes, immunizations, allergies, and surgical, family, and social histories to provide a complete “source of truth” for the patient in the EHR system— completed before the patient’s next visit.
Not all Epic migrations are created equal. That’s why health systems need to engage experts who preserve data integrity, keep patients safe, and keep physicians happy.