Overview
Elevating Health Information Management for Better IT Outcomes
There is a complex landscape of health information management (HIM) best practices to ensure data integrity during major system change. This best practice guide describes how the combination of health information (HI) and information technology (IT) knowledge work together to protect the accuracy of patient data when new EHRs, revenue cycle systems, or other applications are implemented.
Download The HIM Best Practices Guide to Major IT System Change, and learn how to preserve data integrity during EHR, revenue cycle, and other system migrations
Data Quality Challenges in Healthcare: Are We in Denial?
Today, meticulously curated health data stands out as one of the most invaluable assets in the business landscape, impacting both patient safety and the organization’s revenue cycle. While an organization’s EHR ideally serves as the ultimate reference for clinicians, the reality often falls short, directly affecting patient safety and the financial bottom line.

Bad Input Equals Bad Output
In the early 1800s Charles Babbage coined the concept of “Garbage In. Garbage Out.” The acronym, GIGO, became commonplace in the 1990’s as healthcare organizations moved from paper to hospital information systems, EHRs and other digitized data. Interestingly, Babbage’s concept still rings true today.
Poor data quality has a ripple effect, worsening with expanded interoperability and data exchange. The use of faulty data by AI, ML, RPA, and other intelligent tools raises additional industry concerns.
During times of EHR and other IT system change, substantial volumes of data are integrated into your new systems, serving as the foundation for organizational decisions in the years ahead. Data cleanliness is crucial for advancing data usability during these transitions.
An Ounce of Prevention: Why an Effective Strategy and Proper Planning Propel Success
IT systems changes aren’t only about IT. They are about engaging end users and operational teams. These are the staff that will use the new system every day and ensuring their buy-in and adoption is essential. Begin your preplanning and strategy with this reality in mind.

Perform preliminary planning by referencing interview notes and existing guidelines for the initial phase of any system change.
- Identify and implement best practices for this stage.
- Define the consequences of hasty decisions.
- Ensure all stakeholders know the long-term repercussions of inaccurate data.
Craft a comprehensive strategy to support better data quality within your upcoming EHR or other system implementation.
- Prioritize preparedness and resource planning, including operational readiness.
- Implement effective project governance following a Lean methodology.
- Ensure meticulous migration and validation of legacy data.
- Emphasize a talent-driven approach to assembling your team.
- Identify key performance indicators (KPIs) that directly influence cash flow and implement checks and balances to safeguard them.
Empower Your Operations Teams: Harness Expertise and Insights from Diverse Perspectives
Department managers should entrust specific strategic planning needs to individuals closely involved in the processes. These individuals possess valuable insights and awareness of potential pitfalls. They understand what a project might lack and which milestones to incorporate.

Ensure that end users perceive themselves as active collaborators with your implementation team. Otherwise, they may feel that change is being imposed upon them by IT.
Trainers play a pivotal role in frontline testing and may require approval from their supervisors to allocate time from their regular duties to support the project. Often, these individuals are among your most capable and engaged employees.
Tap into subject matter teams or external experts with proven experience across various systems. These seasoned individuals have accumulated a wealth of valuable lessons that can be applied to your project.
Large Northeast Regional Health System Achieves Success with e4health
- Used six-phase process to migrate entire health system to Epic.
- Merged and/or validated 400 downstream systems.
- Addressed 2.7M duplicate tasks.
- Achieved a duplicate rate below 2.5%
- Maximized the value of clean, integrated patient data.
“Early participation ensures the training team is well informed, understand the workflow, and execute an effective training plan. Their in-depth involvement ultimately leads to smoother system transitions and improved patient care.”
– St. Joseph’s Health
It Takes a Village: Cross-functional Teams Deliver Better Results
Valuable Roles for HI Professionals During System Change
- Data Integrity Guardians: Ensure data accuracy and completeness, rectify discrepancies, and maintain high-quality information.
- Clinical Data Specialists: Focus on clinical relevance, bolster trust in data, and reduce clinical errors.
- Data Migration Experts: Oversee precise data transfer to prevent loss or inaccuracies.
- Change Management Champions: Enhance user adoption through training and addressing concerns.
- Data Governance Leaders: Establish standards, policies, and compliance for data quality and management.
Opting for upfront data cleansing takes more time initially, but this best-practice step leads to happier clinicians and bolsters end-user efficiency.
The compelling need to involve health information management know-how during IT transitions becomes apparent as the healthcare industry transitions to fully digitized records, automated processes, and ubiquitous data sharing. The entire healthcare ecosystem will rely on your new EHR information. Therefore, a strong upfront emphasis on data quality and integrity by HI professionals is mandatory for long-term success.
While short-term decisions aimed at trimming implementation costs are tempting, they can jeopardize data quality for years to come.
Strategies to Safeguard Revenue and Mitigate Cash Flow Risks
From a financial perspective, it’s imperative that revenue cycle users are well prepared for new system use on day one. Specific training is an absolute necessity alongside comprehensive system documentation for every detailed step in the patient accounting process.
e4health’s proven success in system migrations, conversions, and implementations is directly attributed to the highest levels of training, testing, and meticulous validation we provide including assurance that users can:
- Drop a claim for every type of encounter and payer.
- Verify the presence of all correct data elements on the claim.
- Ensure smooth dunning cycles to support the processing of multiple claims.
- Confirm that payment posting occurs for all types of claims within the new system.
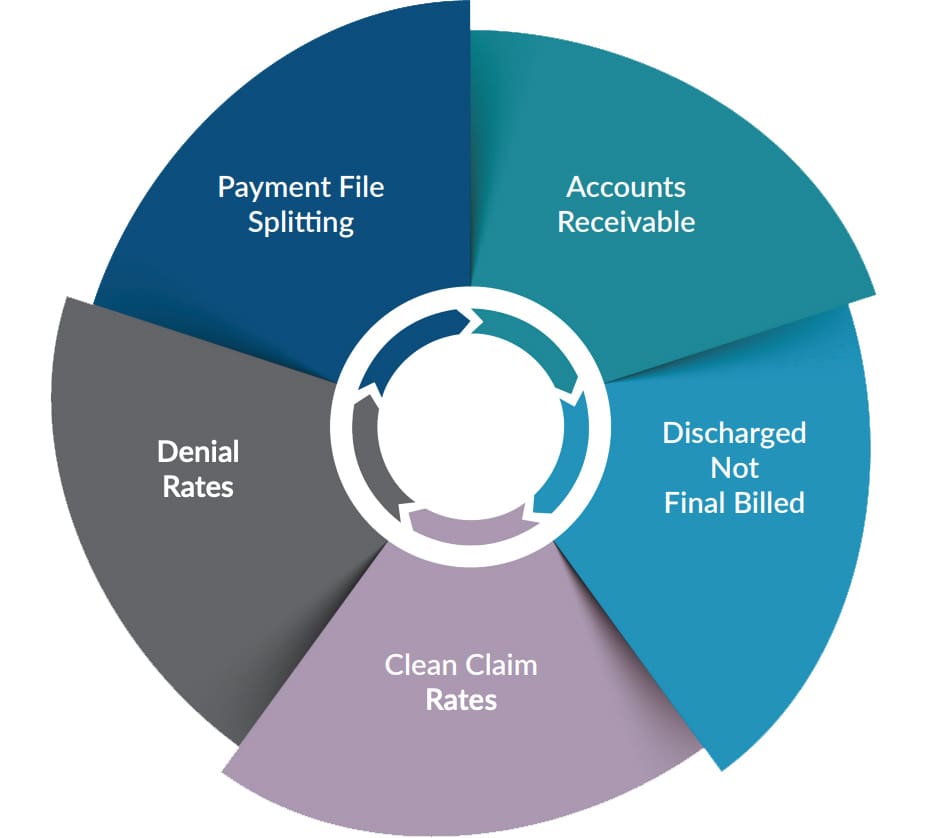
Keep a Close Eye on Your KPIs: Stay Vigilant and Proactive
While it’s true that every major IT system change can have a notable impact on an organization’s cash flow, it’s crucial to understand that this impact can be managed and mitigated. By fostering collaboration across clinical, technical, financial, and revenue cycle departments, organizations can navigate these changes effectively.
This approach becomes even more critical as it helps avoid dramatic spikes in accounts receivable (AR) or claim denials, which can have a detrimental effect on both patient care and financial stability.
To guide you through this process, here are the five most important Key Performance Indicators (KPIs) to monitor during major system transitions and platform upgrades, ensuring a comprehensive understanding of the impact and facilitating a smoother transition.
Ten Common Mistakes During Major System Change
System transitions often highlight the challenge of data duplication across multiple systems. While resolving these issues is crucial, it’s equally vital to consider a frequently overlooked key performance indicator (KPI) – the ‘people factor.’
Our experience shows that system integration reveals not just data integrity issues but also the critical role of the human element. This includes evaluating your team’s adaptability, teamwork, ability to handle change, and the effectiveness of your change management strategies. Ignoring these aspects can lead to negative outcomes.
In system transitions, effective governance should play a more prominent role, ensuring efficient management of both technical and human aspects. This is especially important in an environment where data duplication rates can reach up to 25%, sometimes resulting in staggering numbers, like 800,000 to 1.2 million duplicates within a single health system.
A holistic approach, addressing both data management and team dynamics, is essential for a successful and sustainable system transition.
Did you know?
- Up to 50% of all technology projects require massive rework after launch. Among EHR projects, estimates reveal similar rates.
- 20% of EHR system installations could be considered a failure.
- Negative consequences occur up to 70% of the time, including delays, failed goals, or complete abandonment of the project.
To navigate these complexities successfully, adopting a proactive stance that anticipates potential issues and risks throughout the transition process is crucial.
Standard Slip Ups to Know
1. Fail to prioritize HI’s custodial responsibilities for the legal, electronic medical record.
2. Lack safeguards for crucial KPIs, such as revenue cycle metrics, during significant transition periods.
3. Neglect to conduct data tests, validations, and audits following the migration process to guarantee the integrity of data transferred into the new EHR or other system.
4. Forego proper clinical communication regarding the additional time needed to access and correct line-item data and assess its clinical relevance during patient encounters if clinical data specialists aren’t engaged.
5. Underestimate the financial and temporal investments required for the complete migration of all data to the new system, compared to the alternative of accessing legacy information or data through a different platform or portal.
6. Ignore the equilibrium between legal record and data retention obligations versus the clinical significance of patients’ long-term historical information.
7. Make broad initial decisions regarding data migration and archiving, instead of employing a targeted approach. Migrating all data without discrimination proves to be counterproductive (e.g. irrelevant lab results).
8. Miscalculate the importance of legal health record retention and access requirements for subsequent functions, such as fulfilling information requests, undergoing payer audits, and conducting quality studies.
9. Short-staff patient data duplication and data validation efforts once information is electronically merged or manually abstracted into the new system.
10. Discount new, intelligent technology options for seamless system integration and long-term data integrity maintenance.
New Intelligent Technology Tools Propel Process Efficiency
Strategic collaborations with intelligent technology companies specializing in EHRs, eMPI, and revenue cycle management are instrumental in shaping an effective system strategy. Actively seek out innovative technologies to automate chart and data reviews, identify and eliminate duplicates based on predefined rules, and provide actionable recommendations to clinical data teams.
Why is intelligent technology important?
The emerging capabilities of artificial intelligence (AI), machine learning (ML), and robotic process automation (RPA) will revolutionize legacy data handling. Alliances with these tools drive efficiency, boost productivity, accelerate cash, reduce the burden on healthcare providers, and lead to tangible financial benefits. However, the success of these tools hinges on data accuracy. Simply installing cutting-edge technology upon faulty data is akin to flying a plane without enough fuel. It won’t go very far.
Three areas for HI consideration
- eMPI
- Autonomous Coding
- CDI
Distinguish between myth and reality
There is a significant difference between true AI solutions and ML or RPA. For example, many autonomous coding solutions prioritize high-volume, easily automatable tasks, often neglecting the complexities of inpatient coding. To make informed decisions, it is crucial to differentiate between genuinely intelligent systems and those relying on automated rules alone.
Not all solutions are right for every organization
At e4health, our mission is to meticulously evaluate the growing number of intelligent technologies and ensure the right solutions find their way into the hands of the right customers. We tailor technology choices to individual needs, empowering healthcare organizations to harness the full potential of intelligent systems.
Four Valuable Steps for Data Quality: Data Migration and Validation for The Win
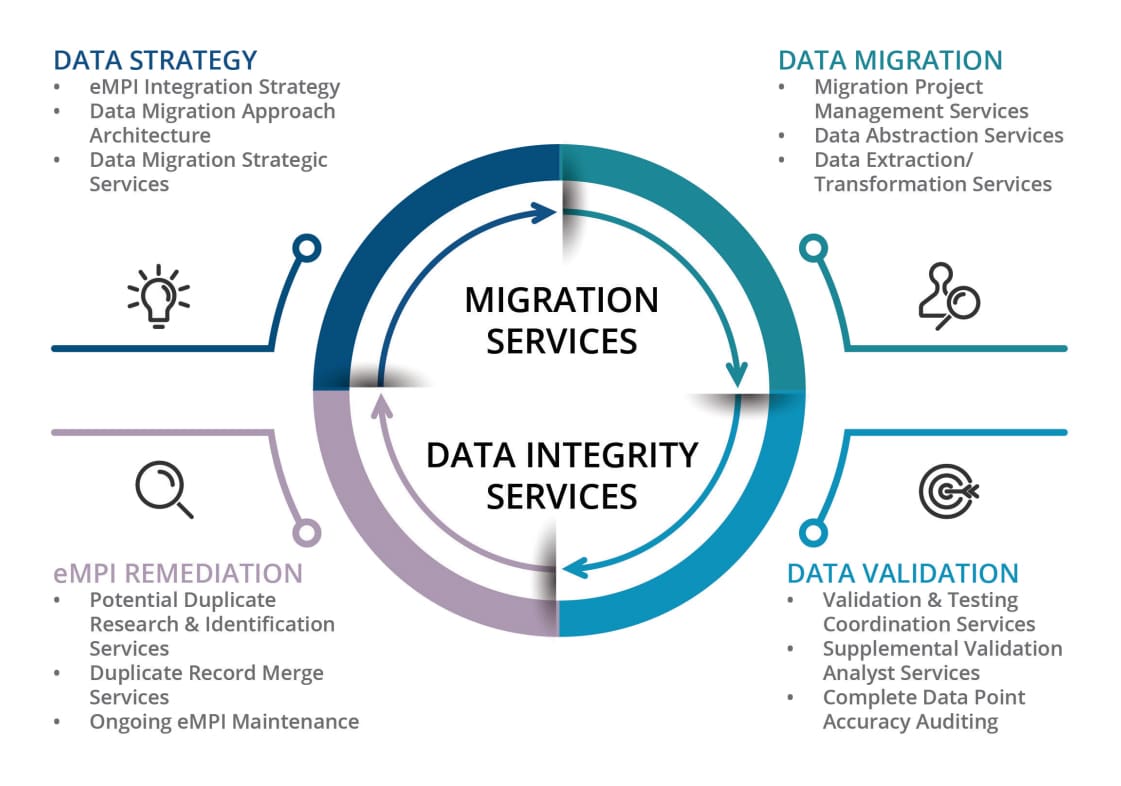
eMPI remediation and ongoing maintenance.
Arm your organization with e4health’s investigative and decision-making skills to ensure a clean and consistent eMPI.
Clinical data abstraction.
e4health’s clinical data abstraction specialists include skilled RNs and credentialed HI professionals deploying proven methodologies to construct a complete clinical picture.
Legacy data migration and validation.
Only e4health possesses the unique combination of HIM and IT subject matter experts and solutions to protect data integrity.
Five Key Inquiries for Assessing a Prospective Partner’s Expertise
1. What project management methodologies do you use?
2. Which systems and versions have you successfully converted in the past?
3. Have you contributed to data migration in both inbound and outbound scenarios?
4. Could you share the typical duplicate rate observed among your customers following the implementation of a new system?
5. Do you include clinicians within your data management team? If yes, could you elaborate on the titles and types of clinicians involved?
The Future of Data Integrity in Healthcare Is Collaboration
e4health is all about blending decades of healthcare information knowledge with our trusted IT system expertise. Our pledge is to empower healthcare information professionals as they embrace the exciting, technology-driven roles that are crucial to reaching healthcare’s future data goals.
In the dynamic world of AI, where there’s no shortage of excitement and advancements, it’s important to remember that we’re still in the early stages of this journey. Every day, we put our commitment into action by injecting fresh ideas and insights into the automation and digitization of healthcare.
These five guiding principles shape everything we do to safeguard data integrity and enhance data quality in healthcare.
Predict new and emerging impacts on data quality.
Protect data quality through proven best practices in HI and IT.
Elevate technical skills for all stakeholders and cross-functional teams.
Stay at the forefront of effective project management methodologies.
Employ intelligent technology to consistently improve efficiency and outcomes.
“As clinicians stepping into EHR testing, it was excellent to have the knowledge of a trainer to help us understand if we had a failed scenario, needed to investigate a potential problem for the future system, or simply lacked sufficient end-user knowledge.”
– MidHudson Regional Hospital
Six Practical Ways HIM and IT Work Together During IT Change
1. Innovate algorithms for discerning low and high thresholds to identify duplicates effectively.
2. Implement automated workflows to ensure HIM experts review potential duplicates.
3. Employ data analytics to quantify the accuracy percentage of data as a crucial system go-live metric.
4. Develop a protocol for the manual transfer of data that cannot be electronically converted.
5. Integrate Lean methodologies to streamline team efficiency.
6. Collaborate with clinicians to validate decisions.
Clinical Data Excellence Is a Journey
e4health understands data integrity is not a once and done event. It is an arduous journey that requires commitment, diligence, and experience. By connecting HI and IT knowledge sets, your organization receives personalized, end-to-end services that encompass the entire clinical data landscape.
Your EHR and other IT systems are important enterprise-wide investments. We ensure their long-term accuracy and success. Read how e4health empowers better health at: e4.health/resources