The audit landscape has changed
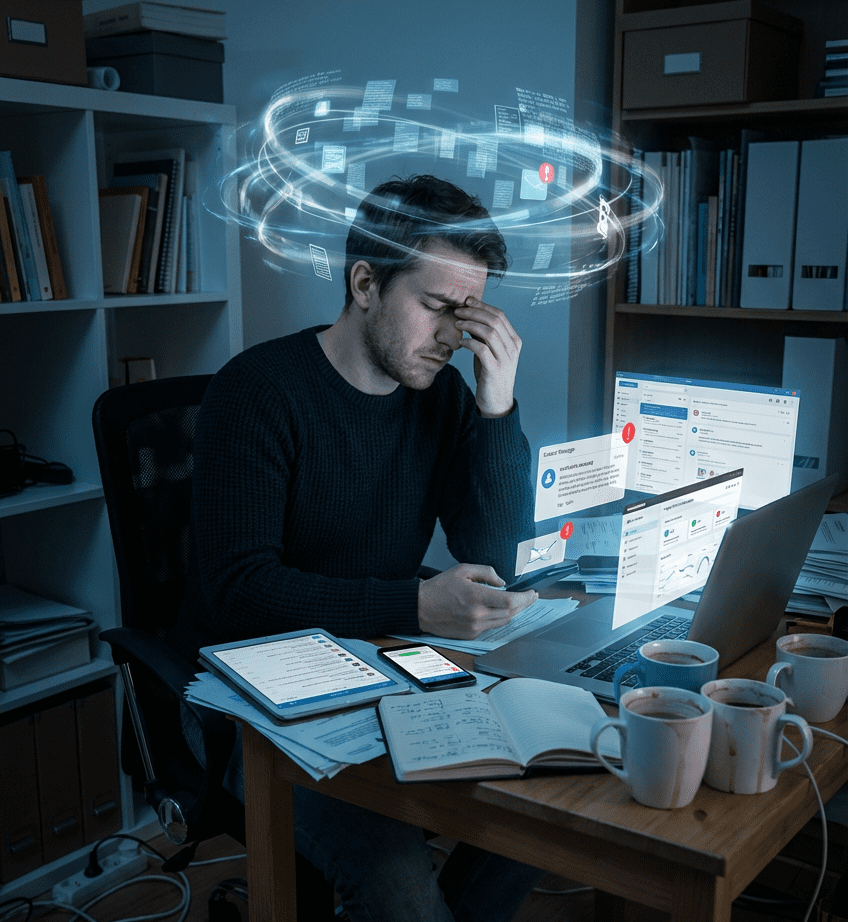
Health Information Management (HIM) leaders are navigating an increasingly challenging audit environment defined by rising denial volumes, more sophisticated payer analytics, and a growing focus on clinical validation. Where denials once centered on technical errors such as missing signatures or incomplete forms, today’s disputes often question the clinical legitimacy of diagnoses that carry significant reimbursement weight.
Organizations are seeing frequent challenges to conditions such as sepsis, severe malnutrition, acute respiratory failure, encephalopathy, and mechanical ventilation hours. These are nuanced areas where clinical interpretation varies, documentation may be inconsistent, and coding decisions are closely scrutinized.
Even when documentation is adequate, payer interpretations do not always align with clinician judgment, leading to prolonged appeals, expensive administrative burden, and unpredictable revenue-cycle delays. A noteworthy portion of these denials are overturned on appeal, revealing inconsistencies in payer decision-making and highlighting the operational inefficiency of addressing documentation weaknesses after the claim has been submitted. For HIM leaders, this landscape reinforces the need for documentation that is clear, specific, and defensible from the outset.
High-risk diagnoses are continuous priorities
Within this evolving environment, a narrow set of high-risk diagnoses consistently emerges as audit hotspots because of their significant impact on DRG assignment and claim reimbursement. Sepsis remains a top target due to differing definitions and the subjective nature of clinical criteria application.
Severe malnutrition is often questioned because of historical concerns around insufficient supporting evidence, while respiratory failure and encephalopathy frequently hinge on how providers articulate clinical findings and reasoning. Mechanical ventilation hours, meanwhile, carry substantial financial implications and are highly vulnerable to documentation gaps in start and stop times.
Given the recurrent nature of these high-risk conditions, organizations must treat them not as occasional points of focus but as continuous priorities requiring ongoing education, second-level review, and real-time monitoring. “Audit readiness” for these diagnoses is not a periodic activity—it is a sustained operational posture.

Shift from reactive denial work to proactive documentation improvement
For organizations seeking to reduce vulnerability to denials, strengthening documentation before a claim ever reaches a payer is essential. Many HIM departments are shifting from reactive denial management to proactive documentation improvement by standardizing compliant query practices, creating targeted tip sheets for high-risk diagnoses, and implementing focused pre-bill reviews for clinically complex cases.
These pre-bill interventions help identify gaps before they escalate into denials and ensure coders and CDI specialists have clear, consistent guidance. Regular denial huddles that bring together CDI, coding, and revenue-cycle teams transform payer trends into actionable insights and provide a mechanism for continuous feedback to providers. Over time, this approach fosters a more defensible documentation culture and reduces avoidable administrative burden.
Provider engagement is the difference-maker
A critical component of audit readiness lies in effectively engaging providers. Physicians often express frustration with traditional documentation education, characterizing it as time-consuming, overly technical, or insufficiently tailored to their clinical context. Successful HIM leaders recognize that meaningful provider engagement requires a shift in education style.
Training is most effective when it is individualized, grounded in examples from the provider’s own documentation, and delivered in small, manageable segments. Micro-learning opportunities—targeting a single concept in under ten minutes—not only respect provider time but also distill documentation expectations into clear, actionable guidance.
Just as importantly, providers are far more responsive when documentation feedback is framed not as a coding requirement but as a driver of care quality, operational efficiency, and reduced administrative burden. When they understand that improved clarity leads to fewer queries, faster billing, fewer denials, and smoother care coordination, providers view documentation improvement as an asset rather than an obligation.

Build durable change with tone and trust
Creating durable change in documentation habits also depends heavily on tone and trust. Providers are more likely to engage when audit findings are presented as opportunities for improvement rather than punitive critiques.
HIM leaders who incorporate before-and-after documentation examples, clearly demonstrate the impact of documentation changes, and maintain a respectful, collaborative approach foster a culture in which providers feel supported rather than scrutinized. This collaborative tone improves both the effectiveness of education and the accuracy of future documentation.
Design pre-bill audits for accuracy without slowing billing
Designing a pre-bill audit program that effectively balances accuracy with efficiency is another cornerstone of audit readiness. The most successful programs are not broad, labor-intensive efforts to review every chart; instead, they target high-risk encounters with the greatest potential financial impact.
By focusing attention on diagnoses that payers scrutinize most closely—such as sepsis or respiratory failure—HIM teams safeguard compliance without creating bottlenecks that slow down the billing process. To ensure such programs deliver value, audit findings must be captured consistently, communicated clearly, and tracked over time through accessible dashboards and analytics. These insights transform audit findings from isolated events into a continuous improvement mechanism that strengthens broader operational processes.

A minimum viable model can still deliver strong ROI
Even organizations with limited resources can implement high-value audit oversight by adopting a minimum viable pre-bill audit model. This may involve reviewing a small number of high-risk charts each week, rotating audit topics monthly based on denial trends, and conducting short interdisciplinary huddles to discuss findings.
When framed appropriately, even small audit programs yield substantial financial protection. For example, a sample review of 100 high-risk encounters may uncover $35,000 in preventable financial impact while requiring only $4,125 in labor—yielding an ROI of more than 740%. Such tangible outcomes make it easier for HIM leaders to justify audit investments to executives motivated by productivity concerns.
Use data to anticipate payer behavior
As audit programs mature, data becomes a critical tool for predicting and preventing payer disputes. A well-structured dataset—even a spreadsheet—can track payer behavior, provider-specific documentation patterns, financial impact, agreement or disagreement with payer rationale, and appeal outcomes.
When organizations cross-reference denial data with query trends, they can identify documentation vulnerabilities before they manifest as denials. This proactive, data-driven approach moves organizations from responding to payer activity to anticipating it, strengthening long-term revenue protection and operational resilience.

Align CDI and coding to present a unified story
Collaboration between coding and CDI teams further amplifies audit readiness. When these functions operate from different policies, varying interpretations, or inconsistent query practices, payers may perceive documentation as unreliable or contradictory.
Organizations that present a unified, consistent approach—backed by shared query standards, aligned educational materials, joint case reviews, and integrated reporting—are better positioned to defend their claims. Centralized technology platforms and shared repositories of reference materials help ensure this alignment remains intact even across remote or multi-facility teams, creating a single source of truth that supports decision-making.
Translate audit risk into executive-ready language
Equally important is HIM’s ability to communicate audit risk effectively to executive leaders. Executives do not require the technical intricacies of coding guidelines; they need a clear understanding of how documentation patterns, denial trends, and payer behaviors influence financial performance and compliance exposure.
HIM leaders who translate complex findings into concise visuals, trend summaries, and narrative explanations create clarity and confidence. Pairing every identified risk with a clear mitigation plan reinforces credibility and demonstrates organizational control. Regular, structured updates help sustain trust and elevate HIM’s role as a strategic contributor to revenue integrity and operational resilience.

Build a resilient HIM workforce for long-term readiness
Sustaining high performance in this increasingly complex environment also requires building an adaptable, resilient HIM workforce. The pace of payer change and the complexity of audit methodologies can create fatigue, especially if audit findings are perceived as punitive.
HIM leaders who cultivate a culture of psychological safety—where errors are viewed as learning opportunities rather than failures—encourage staff to openly discuss challenges, ask questions, and provide feedback. Micro-learning, transparent communication about payer trends, and recognition of improvement help staff stay informed and motivated. Over time, this culture of continuous learning strengthens team agility and builds long-term readiness for evolving payer scrutiny.
Conclusion
In an era defined by rising clinical denials, increasing complexity, and heightened financial risk, audit readiness has become a strategic imperative rather than a compliance exercise. Organizations that succeed will be those that weave documentation integrity, clinical collaboration, targeted audit oversight, data-driven insight, and adaptive leadership into a coherent operational framework.
When HIM leaders strengthen provider relationships, align internal teams, leverage actionable data, and foster resilient, informed staff, they transform audit readiness from a defensive necessity into a competitive advantage. The goal is not merely to avoid denials—it is to build a high-performing ecosystem where accuracy, clarity, and financial protection thrive together.